Wednesday, July 30, 2008
Understanding Osteopetrosis
1150 17th St., NW, Suite 500, Washington DC 20036
202-223-0344 or 800-624-BONE
TTY (202) 466-4315
E-Mail: orbdnrc@nof.org
One of the less common metabolic bone disorders is osteopetrosis. Osteopetrosis is an inherited disease caused by a defect in bone resorption--the process in which old bone is broken down and removed so that new bone can be added to the skeleton. Osteoclasts are the cells responsible for bone resorption. In osteopetrosis the osteoclasts do not perform normally, either because there are too few of them or because they are ineffective in removing bone. This flaw in bone resorption results in bones that are abnormally dense, yet are easily broken. Men and women are equally affected by the disease.
The increased bone mass in individuals with osteopetrosis can limit the amount of available bone marrow space. Since the bone marrow is responsible for the production of blood cells, impaired bone marrow function can produce several clinical problems. For example, interference with red blood cell production can lead to anemia. Impairment of white blood cell production can limit the body's ability to fight infection. When platelet production is suppressed, individuals are prone to bleeding since platelets are essential for clotting blood. Anemia, infection, and bleeding are just some of the symptoms that individuals with osteopetrosis can experience--blindness, deafness and even stroke can occur when the skeletonis so dense that blood vessels and nerves cannot pass through the bones.
Three major types of osteopetrosis have been identified in humans:
Malignant infantile form. This type of osteopetrosis is usually discoveredin the first months of life. In addition to having many of the above symptoms of the disease, children with this condition often have significant delays in psychomotor and tooth development. The malignant infantile form of the disease can be severe and frequently results in death from infection or bleeding. In fact, thirty percent of children with this form of the disease will die during the first ten years of life. This form of the disease is inherited as an autosomal recessive trait—there by affecting some brothers and sisters.
Adult form. The adult form of osteopetrosis is milder than the infantile form. This type of the disease is benign and generally does not alter life expectancy. Many of the individuals with the adult form of osteopetrosis have few or no symptoms. It is inherited from generation to generation as an autosomal dominant trait.
Intermediate form. This type of the disease is found in children younger than ten years of age. It tends to be less severe than the malign antinfantile form, but more severe than the adult form. Individuals with this type of osteopetrosis generally do not have a reduced life expectancy.
The diagnosis of osteopetrosis is usually made when dense bones are discovered on x-rays. A bone biopsy can confirm the presence of the disease, while supplemental tests are usually performed to evaluate any potential complications. Confirming the specific subtype of the disease is important so that individuals can receive the most appropriate treatment.
Various therapies have been used in the treatment of osteopetrosis. Bone marrow transplantation (BMT) allows the abnormal osteoclasts to be replaced with normal cells. BMT is the only approach that has resulted in a cure of the malignant infantile form of the disease. Because of its high failure rate and because of its side-effects, BMT tends to be reserved for only the most severe cases of osteopetrosis. According to the Paget Foundation, survival rates after BMT in children with osteopetrosis range from 40-70%.
High doses of calcitrol (the active form of vitamin D) have been used tostimulate osteoclast function in individuals with osteopetrosis. Calcitrolhas been shown to significantly reduce symptoms in people who have mild or severe forms of the disease, though it is not approved by the Food and Drug. Administration for this purpose. Similarly, experimental use of interferon gamma 1-b treatment has been reported to decrease infection rate and improve blood abnormalities in severely affected patients. Another type of medication that may be used to treat patients with osteopetrosis are glucocorticoids. Large doses of glucocorticoid drugs (such as prednisone) may be given for short periods of time to patients with impaired red blood cell or platelet production.
Research efforts are underway in an attempt to identify the gene defects that cause osteopetrosis.
Two documents on osteopetrosis have recently been developed by the Resource Center and the Paget Foundation: a patient information brochure and an annotated bibliography for professionals. For further information on these educational resources, please contact the ORBD~NRC at 202-223-0344.
Monday, July 14, 2008
Gene Research Heightens Hope for Curing Autism
15:17, July 13th 2008
http://www.efluxmedia.com/news_Gene_Research_Heightens_Hope_For_Curing_Autism_20270.html
U.S. researchers have found six new genes involved in autism. More exactly, they found that these genes are responsible for new brain connections needed in the process of learning.
What was really impressive was that these genes were turned off and their silence places them among many mutations that lead to the devastating disorder. Finding ways to turn them on might lead to curing autism, according to the study’s authors.
Autism is a spectrum of different disorders ranging in severity and in symptoms from the mild Asperger’s syndrome to more severe autism. The disease, characterized by poor social interactions, impaired communication and repetitive behavior, affects as many as 1 in every 150 kids in the U.S., according the Centers for Disease Control and Prevention.
For the study, Dr. Christopher A. Walsh and Dr. Eric Morrow of Harvard Medical School in Boston and colleagues analyzed 104 Muslim families from a series of Middle East countries, in which there was a high incidence of autism. In Middle East countries, there is an increased tendency for cousins to marry, raising kids’ odds of inheriting rare mutations. There were 88 such families involved in the study.
The genetic analysis of these families revealed that autism is not only caused by the deletion of some genes but also by turning off other genes. These particular genes cause disruptions in the brain’s ability to form new connections in response to experience.
The good news is that these genes involved in autism were just turned off and not deleted. Now the only thing that researchers need to do is to find ways to turn these genes on in order to improve and eventually cure autism.
"Interestingly, not all the affected genes were actually deleted, but only prevented from turning on, offering hope that therapies could be developed to reactivate the genes," the researchers wrote in the July 11 edition of the journal Science.
Autism Treatment Study
CBS 42 News 2008-07-11 16:55:07.0
http://www.cbs42.com/news/local/24540294.html
Birmingham HBOT is the only treatment center in Alabama offering large pressurized tanks used to immerse the brains of autistic children in oxygen, to try to reverse some of the effects of the disease.
Now, some children undergoing hyperbaric therapy are also being treated for toxic metal exposure with a treatment called chelation. "Chelation is basically using either natural or drugs to remove either lead or mercury," said Dr. David Adams. He says the medical community has been slow to accept the treatment due to lack of evidence, but a new study could soon change that. "I think the NIH is listening to parents and listening to parent reports of improvement with chelation and are attempting to scientifically evaluate that," Adams said.
Parents of autistic children say whether you're talking about hyperbaric oxygen therapy or chelation, the medical controversies don't matter as much as the actual results they've seen in their children's lives. "Once we started adding the chelation to it we had a lot of his people that work with him in school, therapists and so forth, really start to see a big difference in how responsive he was," said Rodney Allison. "It's like they've come alive, gradually by gradually I'm getting my kids back cause it was like they died," said Tracey Martin, the director of Birmingham HBOT.
Dr. Adams says children may become exposed to mercury and lead from fish, coal fired steam plants, and certain vaccines.
Sunday, July 6, 2008
Current Health Issues
Symptom
Recurring convulsions following a dreadful (abdominal and/or bone) pain.
Remark
(1) No history of seizures.
Around 10 times seizures have happened in the last 1 year. The last 5 seizures were within 3 days (April 6, 7 & 8, 2008).
(2) The convulsions happen around 2 hours after meal; except:
a. The 7th, 8th & 9th happened when taking a meal (about 5 to 10 minutes after starting the meal).
b. The last seizure happened because of a fear feeling of her blood sample being taken.
(3) The first convulsion (last year) was most likely triggered by her constipation (seemed very hard and painful to pass the faeces).
a. She has suffered from constipation since January 2007 (her colon was full of faeces up to the rectum position).
b. In the beginning, she suffered from a diarrhea (January 22, 2007) and was treated with Smecta & Protexin.
c. The diarrhea was discontinued but her stomach bloated 3 days after the treatment and was given Tilidan, Zantac & Pankreoflat for the first 3 days and Cotazym Cobazym, Becombion & Motilium for the next 7 days. No sign of recovery on her constipation.
d. Later on, Movicol does help her with the constipation and has been given to her everyday for the maintenance up till now.
(4) Note: Since March 2005, she has suffered from osteomyelitis in the right maxilla. The osteomyelitis is repeatedly manifested in a form of a big swell comes out on her right cheek and/or around her right eye.
a. Antibiotic is given to her whenever the osteomyelitis recurs. Antibiotics were given 18 times within 20 recurrence of osteomyelitis for a period of 36 months (March 2005 up to Feb 2008). Recurrence duration has become shorter progressively to one month period.
b. An opening of an abscess in her right cheek was conducted in March 2008. No swell appeared afterward. The incise is still in an open condition (unintentionally) and the pus still drops regularly.
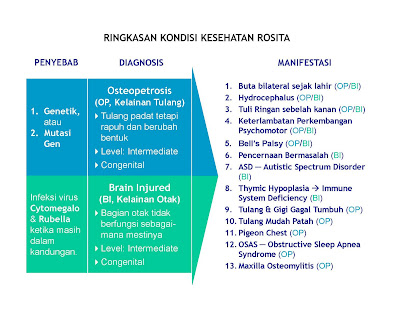
Summary of Diagnosis/Prognosis
(1) Hydrocephalus
a. Non-communicating
· Plug in aqueduct of sylvius
b. Enlargement on lateral and 3rd ventricles
· Suspect tumor presence in 3rd ventricle
(2) Vision Impairment
a. Blind (both eyes)
· No or very little response to light
· Suspect optic nerve damage in central nervous system
· Severe visual impairment because of bilateral optic atrophy which is part of the generalized cerebral atrophy
b. CMV Syndrome (some small dots in retina)
c. Strabismus
(3) Hearing Loss
a. Right mild hearing loss (30–40 dB)
(4) Craniosynostosis
a. Right coronal suture has joined/united
(5) Osteopetrosis
a. Suspected intermediate osteopetrosis
b. No evidence of hepatosplenomegaly
c. No progressive growth of osteopetrosis; normal life expectancy
(6) Rubella Syndrome
a. Radiolucent on all articulations
(7) Gastrointestinal
a. The feces observed proved to be measuring blood
b. Some observations (endoscopy, colonoscopy, meckel scan, bleeding scan) were unable to detect the source of bleeding
c. Gastroenterologists’ recommendation for surgery of exploring ileum has been rejected by patient’s parents
(8) Autistic Spectrum Disorder (ASD)
a. Non-verbal & some developmental disability in behavior
b. Nutrient & potentially toxic elements
· Elevated or depressed level in blood: Calcium, Manganese & Potassium
· Elevated or depressed level in hair: Magnesium, Copper, Zinc, Manganese, Vanadium, Cadmium, Lead, Mercury, Aluminium, Thallium & Tin
(9) Obstructive Sleep Apnea Syndrome (OSAS)
a. Sleep Apnea with Apnea-Hypopnea Index 31,9 per hour
b. Laryngoscopy result showed macroglossae
c. Obliteration of lumen airway
(10) Maxilla Osteomylitis
a. Peritoneal reaction at upper right medial maxillary
b. Recurrent soft tissue swollen around right maxillary; suspected chronic osteomylitis
Milestones
· Apgar score: 10/10
· Blood group: B+, Hb: 18.1 g%, Ht: 58 v%, and bilirubine: 6.7 mg%
· Weight: 2950 gram, length: 49 cm, and head circumference: 34 cm
(2) Since being born, appeared to be reluctant for feeding. Often fell asleep after feeding for about 5 to 10 minutes.
(3) At two-month old, the fontanel’s surface began to rise
(4) First hospitalized on December 22, 1997 (2½ months old) for diarrhea and vomiting
(5) At 2½ months old, she was diagnosed for having been once infected with Rubella and Cytomegalovirus. The optic nerve was also diagnosed to be not vital.
(6) Though at 2½ months old ventricle had been slightly enlarged, the diagnosis of hydrocephalus was just acknowledged at the age of 9 months.
(7) Has 4 teeth at 7 months old, nevertheless no more additional tooth up to now. In fact, 1 tooth fell out at 5½ old years.
(8) Can walk by her self at almost 3 years old (Sep 2000).
(9) Can “sing” with accurate tone up to 3 years old.
(10) Entering the 4th years, her general condition including her communication ability was weakening. Vocabulary was disappearing and bubbling often. She can say words for things she really wants or don’t want.
(11) At April 1, 2002 (4 years & 5 months old) she fell coma for 1 day. Suspected because of obstructive sleep apnea syndrome (OSAS). She was in ICU for 25 days. A ventilator was employed for 4 days to manage her post-laryngoscopy breathing. Since April 2, 2002, a goedel (oropharyngeal) airway should be inserted to her mouth during night-sleeping time to keep the airway opened.
(12) So far, she has been 10 times hospitalized for: gastrointestinal problem, fracture at femur dextral 1/3 proximal, surgery for implanting VP shunt, surgery for inguinal hernia, surgery for VP shunt reposition, fracture at femur sinister 1/3 proximal, fracture at tibia sinistral, OSAS, and several convultions.
(13) Under coordination of pediatric, expertise involved continuously or just considered for second opinion include:
a. Pediatric Neurology
b. Neurosurgery
c. Gastroenterology
d. Ophthalmology
e. Otolaryngology
f. Pulmonology
g. Orthopedic
h. Hematology
i. Pediatric Surgery
j. Radiology
k. Cardiology
l. Medical Rehabilitation
m. Psychiatry
n. ENT
o. Naturopathic
p. Immunoendocrinology
q. Endocrinology
Saturday, July 5, 2008
Tabloid "Nakita" - 178, 2002

Betapa tidak! Anakku dihinggapi berbagai kelainan. Ia buta, hidrosefalus, tulangnya rapuh hingga mudah patah. Bahkan, ia pun sempat mengalami henti napas. Berkat kebesaran-Nya sampai saat ini masih bersama kami, dengan segala keterbatasannya.
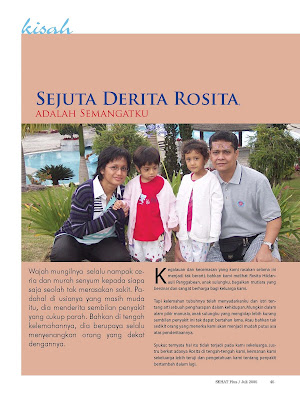
Anak kami, Rosita Hildanauli Panggabean, lahir 16 Oktober 1997 dengan berat 2950 gram, panjang 49 cm dan APGAR score 10/10. Saat itu semua tampak baik-baik saja, demikian pula selama kehamilan, semua tampak normal. Tapi memang, selama kehamilan tersebut kami tidak melakukan pemeriksaan darah. Ini karena dokter kandungan yang menanganinya mengatakan bahwa pada Rosi tidak terdapat indikasi untuk dilakukan pemeriksaan. Kondisi ibundanya pada saat itu dianggap baik-baik saja.
Namun begitu, kondisi normal Rosi mulai berubah saat usianya 2,5 bulan. Ubun-ubunnya mulai tampak agak menonjol dan terlihat "naik". Ini pun kami ketahui secara kebetulan saat ia mengalami diare dan dibawa ke RSAB Harapan Kita, Jakarta. Dokter anak yang menanganinya, sambil menangani diare yang dialami Rosi, justru lebih khawatir dengan ubun-ubunnya yang tidak seperti anak normal.
Pulang dari rawat inap, 24 Desember 1997, kami segera berusaha mencari dokter ahli untuk memeriksakan lebih lanjut keadaan kepala Rosi. Untunglah, ada kenalan yang bisa mengantar kami ke seorang profesor dari bagian kesehatan anak di RSCM, Jakarta. Keesokannya, 25 Desember 1997, walau saat itu hari libur, beliau berkenan memeriksa keadaan Rosi di rumahnya. Beliau mengatakan, Rosi memerlukan pemeriksaan lanjutan di RSCM. Esoknya lagi, 26 Desember 1997, ia diperiksa dengan CT Scan dan EEG, lalu dikonsulkan ke profesor ahli saraf anak, dan belakangan lebih sering dengan dr. Jimmy Passat, Sp.A(K). Oleh mereka diputuskan, Rosi harus dirawat di RSCM selama 3 minggu.
Selama di sana Rosi mengalami macam-macam pemeriksaan dan keadaannya selalu dimonitor. Kami ingat, saat itu dr. Jimmy berkata, perjalanan yang harus dilalui tampaknya akan panjang. Kami seperti tersadarkan bahwa keadaan semakin lama semakin tidak mudah.
Dalam masa itu juga, kami mencurigai adanya kelainan pada mata Rosi. Setelah diperiksa oleh dokter ahli mata, tampaklah saraf mata anak kami ternyata ikut rusak sehingga ia tak bisa melihat untuk selamanya. Diagnosa yang diberikan adalah Rubella Syndrome. Ini didukung hasil pemeriksaan darah yang ternyata menunjukkan Rosi pernah terkena infeksi rubela dan sitomegalovirus (CMV) saat di kandungan. Sejak itu pemeriksaan difokuskan pada Rubella Syndrome dan CMV. Syukurlah, ternyata jantung Rosi tidak ikut mengalami kelainan.
KELAINAN TULANG
Cobaan belum selesai karena sebelum sampai usia 1 tahun, Rosi mengalami patah tulang pada paha kanannya hanya karena jatuh yang ringan. Melalui berbagai pemeriksaan, akhirnya diketahui Rosi juga menderita kelainan pertumbuhan tulang yang disebut osteopetrosis. Inilah yang menyebabkan tulangnya mengalami penebalan, perubahan bentuk, dan mudah patah.
Satu-satunya pengobatan yang ada saat ini untuk osteopetrosis adalah dengan transplantasi sumsum. Namun karena menurut tim dokter osteopetrosisnya masih dalam kategori moderate, dan risiko komplikasi transplantasi juga besar, dikatakan bahwa transplantasi belum perlu dilakukan.
Akibat osteopetrosisnya inilah, hingga kini Rosi sudah mengalami patah tulang sampai 3 kali, hanya karena sedikit terbentur atau jatuh ringan saja. Belum termasuk beberapa retak tulang di selangka dan rusuk yang kami ketahui belakangan. Bahkan kini ia didiagnosa mengalami kelumpuhan salah satu saraf di wajahnya, karena ada saraf yang terjepit oleh tulangnya sendiri.
Menjelang usia 1 tahun itu pula, Rosi didiagnosa hidrosefalus dan harus dioperasi untuk memasang VP shunt di kepala. Alat ini diperlukan untuk mengatasi hidrosefalus yang dideritanya. Belakangan, saat berusia sekitar 1,5 tahun, alat ini mengalami kerusakan dan tidak berfungsi dengan baik, sehingga Rosi harus menjalani operasi lagi di kepalanya untuk memperbaiki posisi VP shunt.
GANGGUAN NAPAS SAAT TIDUR
Belakangan, saat Rosi berusia sekitar 2 tahun, kami melihat ada masalah dengan pernapasannya. Rosi jadi mengorok saat tidur dan makin lama tampak makin parah. Bolak-balik kami ke dokter ahli paru, namun tak ada perbaikan. Akhirnya setelah kami mencari-cari melalui internet,kami curiga Rosi menderita kelainan bernapas saat tidur yang disebut Obstructive Sleep Apnea Syndrome (OSAS). Akibat OSAS ini, bila Rosi tidur, ia mengalami kesulitan bernapas, bahkan hingga menjadi biru.
Untunglah, dokter yang saat ini menangani Rosi, yaitu dr. Hardiono D. Pusponegoro Sp.A(K) memahami tentang OSAS yang dialami Rosi. Kelainan ini memang termasuk langka di Indonesia. Rosi kemudian diperiksa di sleep laboratorium untuk mengetahui secara pasti keadaan OSAS-nya. Bersamaan dengan itu, ternyata kondisi Rosi memburuk, hingga akhirnya Rosi harus dirawat di ICU anak di RSCM selama 25 hari, sejak 1 April 2002.
Selama berhari-hari menunggui Rosi di rumah sakit, kami kembali berpikir, apa, sih, yang menjadi rencana Tuhan untuk Rosi dan untuk kami? Ketika ia terbaring koma dan dokter membatalkan semua tindakan medik yang sudah direncanakan, kala itu kami benar-benar "jatuh" dan merelakan Rosi untuk "pergi".
PEMULIHAAN LUAR BIASA
Kini Rosi sudah berada di rumah sejak 25 April 2002 lalu. Kami semakin percaya bahwa Rosi memang anak kesayangan-Nya. Dari kondisi di mana ia sempat tak sadarkan diri, tak bisa bernapas tanpa bantuan ventilator dan 3 minggu harus makan lewat selang di hidung, kini Rosi dapat bernapas sendiri dengan tingkat kesadaran penuh. Free at last! At home! Di rumah ia cukup berbekal gudel (alat kecil yang harus dipasang di mulut selagi tidur untuk membantunya bernapas).
Uniknya, setelah dirawat di ICU itu Rosi mulai mau "bernyanyi" lagi. Lagu-lagu yang dulu sering ia nyanyikan kini sudah bisa ia dendangkan lagi sepotong-sepotong. Bahkan lagu yang tidak pernah ia nyanyikan, sekarang ia nyanyikan. Entah apa penyebabnya sehingga ia bisa pulih luar biasa seperti itu. Barangkali karena selama dirawat di RS, walaupun kondisinya antara sadar dan tidak, kami terus memutarkan lagu-lagu kesayangannya, sehingga mungkin itu semua terekam dalam otaknya. Memang ia masih belum bisa berkomunikasi secara verbal, jalannya masih tertatih-tatih, masih suka jengkel dengan memukul kepalanya sendiri. Namun, ia sudah bisa makan melalui tenggorokannya makanan yang mesti diblender seperti biasanya.
Kami saat ini merasa tidak layak tahu apa kehendak Tuhan. Kami mau memikul apa yang diharuskan-Nya untuk kami pikul. Kami percaya Rosi juga demikian, meski apa yang ia rasakan jauh melebihi yang kami rasakan. Melalui kehadiran Rosita, kami belajar hal penting bahwa rancangan kami bukanlah rancangan-Nya.
Sewaktu belum menikah dulu, kami sering berangan-angan bahwa kalau punya anak nanti, pada saat usianya 1 tahun ia akan kami ikutkan kursus renang. Pada usia 3 tahun, ia akan kami masukkan ke kursus Kumon dan mulai "sekolah" di taman bermain.
Pada kenyataannya Rosi tidak ikut kursus renang sampai sekarang. Namun, ia senang sekali bila diajak berenang walau awalnya menunjukkan rasa waspada. Kalau sudah begitu, ia selalu bilang "cipak-cipuk". Pun, pada kenyataannya ia tidak ikut kursus Kumon dan tidak ikut taman bermain di usia 3 tahun, tapi ia sudah mulai belajar di Pelayanan Dini sekolah khusus tunanetra/dwituna "Rawinala" dan "BRT" (Bimbingan Remedial Terpadu) pada usia 2 tahun.
Banyak yang didapat Rosi terutama dari segi bina diri dan kemampuan bersosialisasi. Ia kini sudah mampu memakai baju sendiri, juga memegang sendok sambil makan. Ia pun mulai mengerti perintah-perintah pendek seperti, "Mari duduk", "Berdiri". Hal yang biasa bagi anak normal. Rosi juga amat senang "bernyanyi". Lagu favoritnya adalah "Tennesse Waltz" dan "Bangun Tidur".
ROSI MENGAJARKAN ARTI HIDUP
Seandainya saja Rosi tidak buta, mungkin kami tidak sebersyukur ini kepada Tuhan, serta tidak sesukacita dan sesabar ini dalam menanti hari demi hari ataupun tetes demi tetes kemajuan anak-anak kami. Melalui sakitnya yang terakhir, kami juga melihat bahwa begitu banyak orang di sekeliling kami yang mengasihinya. Kami berharap mereka bukan sekadar tersentuh oleh ketidakberdayaan Rosi dan kami, melainkan oleh kesadaran untuk dapat lebih menghargai kehidupan kanak-kanak yang normal, yang "bawel" karena dapat melihat, yang berlarian ke sana-ke mari karena kaki yang kuat, dan yang dapat bernapas dengan lancar tanpa perlu bantuan peralatan apapun.
Saat ini kami tetap tak tahu sampai kapan Rosi bisa bertahan. Namun, kami selalu berusaha memberikan yang terbaik baginya. Kami melihat ada rencana dari Yang Maha Kuasa yang harus kami jalani, entah apakah rencana itu. Namun kami yakin, rencana-Nya ini adalah rencana yang baik bagi kami.
Martin Leman (seperti dituturkan Sahat Panggabean dan Grace Pelawi, orang tua Rosita Hildanauli Panggabean.e-mail: rositapanggabean@gmail.com.) Foto:Dok.Pribadi